Tendons
Tendon injuries and pain are common amongst athletes of various sports and ages. Tendons attach muscle to bones and allow muscles to transmit force across our joints which allow us to move, walk, run and jump!
Tendons most commonly become injured when they undergo a period of loading above and beyond what they are used to. We call these injuries Tendinopathies and they have been shown to have a continuum of dysfunction ranging from reactive to degenerative, or more commonly described as acute or chronic (Cook and Purdam 2008). Due to this variability of tendinopathy injuries, management for tendon injuries can be difficult and requires accurate assessment and targeted individualised interventions.
Isometrics
Current research in patella tendons has shown isometric exercise has a place in athletes with pain as it has an analgesic effect (Rio et al 2017). The findings of these studies in patella tendons have been applied for tendons throughout the body in both professional sports and in private practice with the general population. The proposed cause of pain relief with isometrics in these studies is a reduction in pain related muscle inhibition leading to increase in strength and changes to the central nervous system which dampen pain. (Rio et al 2015)
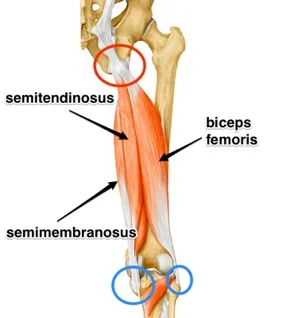
More recently it has been proposed that this widespread adoption of isometrics may not be applicable to tendons throughout the body in areas such as the Achilles tendon, lateral epicondylalgia (tennis elbow) or hamstring tendons (Coombes et al 2016).
Achilles Tendon Anatomy
Muscles That Attach to the Achllies - Gastrocnemius Vs Soleus
There are 3 muscles that attached to the Achilles Tendon. The soleus and the gastrocs are the largest and have the most significant contribution to athletes who run, jump and change direction. The gastroc’s crosses the knee and is a more active in ankle movements when the knee is straight, and the soleus is more active when the knee is bent. The reality is that both muscles are quite different in their location and function, but they both need the be strong and work together to support the Achilles Tendon during sport.
Calf Muscle Anatomy
People with tendon injuries and tendon pain have been found to have weaker calf strength in both the injured and the corresponding limb muscles than other people without tendon pain (O’Neill 2018). Essentially if an athlete does not have the adequate strength in their muscle, their tendon will be required to take on more load. As a result we often see them fail and become painful as they attempt to cope with the excessive loading that the tendon is unaccustomed to. So STRENGTH is the key! But which type???
Other Exercise Therapy
Isotonic (Or through range strength training) strength training, which includes both concentric and eccentric components, has recently been suggested as a more appropriate way to manage tendon injuries other than the patella tendon (O’Neill et 2018). This type of strength training needs to be heavy at around 70-80% of 8RM (repetitions maximum), and must be appropriate to the type and stage of tendon injury as detailed above. In Achilles Tendinopathies the most appropriate exercises are loaded calf raise in seated and standing positions (see pictures below). These should be progressed to single leg variations with load as symptoms and strength allows. Both of these exercises target the major calf muscles of the gastrocnemius and soleus in differing amounts.
*NOTE: These aren’t intended to be pain relieving and need to be prescribed around the athletes training appropriately.
Loaded Standing Single Leg Calf Raise
Loaded Seated Calf Raise
To Isometric Or Not
The type of strength stimulus we put through our tendon and adjoining muscles is extremely important when dealing with injury and needs to be case specific. As mentioned Isometric strength training has been successfully used for tendinopathies in certain areas of the body, and as a result adapted to other areas throughout the body.
However, they are not the only form of resistance training we should expose to an injured tendon, as strength gain’s through ROM are important and functional to the sports that many athletes play. As for the Achilles the focus should be on improving strength in the calf complex relative to the athlete’s sport. This may be a combination of loaded strength rehab and higher velocity power strength work. This ALWAYS needs to be specific to the demands of the athlete’s sport and goals.
Isometric exercises still have an important role in tendon pathology!! But they aren’t the only type of strength to take into consideration when you have any type of tendon pain.
For other general information regarding tendons and in particular patella tendons refer to our previous article published by Luke Heath on our website “Jumpers Knee: Patella Tendiopathy – Diagnosis and Management”.
For any further questions or to book an appointment contact us online or via phone.
Written By Chris Bailey - Titled Sports Physiotherapist and Rehab Specialist
References
· Cook J, Purdam C. Is Tendon Pathology a Continuum? A Pathology Model to Explain the Clinical Presentation of Load-Induced Tendinopathy. British Journal of Sports Medicine. 2009
· Coombes B, Tucker K, Vincenzino B. Achilles and Patella Tendinopathy Display Opposite Changes on Elastic Properties: A Shear Wave Elastograpy Study. Scandavian Journal of Medicine and Science in Sports. 2018
· O’Neill S, Radia J, Bird K, Rathleff M, Bandholm T, Jorgensen M, Thorborg K. Acute Sensory and Motor Response to 45-s Heavy Isometric Holds for the Plantar Flexors in Patients with Achilles Tendinopathy. Journal of Knee Surgey, Sports Tramatology and Arthroscopy. 2018
· O’Neill S. PhysioEdge podcast Episode 82. 2018
· O’Neill S, Watson P, Barry, S. Why are Eccentric Exercises Effective for Achilles Tendinopathy? The International Journal of Sports Physical Therapy. 2015
· Rio E, Kidgell D, Purdam C, Gaida J, Mosely L, Pearce A, Cook J. Isometric Exercise Induces Analgesia and Reduces Inhibition in Patella Tendinopathy. British Jounal of Sports Medicine. 2015
· Rio E, Van Ark M, Docking S, Mosley L, Kidgell D, Akker-Scheek I, Zwerver J, Cook J. Isometric Contractions are More Analgesic than Isotonic Contractions for Patella Tendon Pain: An In-Season Randomised Clinical Trail. Clinical Journal of Sports Medicine. 2017